Arrhythmogenic right ventricular dysplasia
Arrhythmogenic right ventricular dysplasia is a rare form of. Patients with this pathology will have fibrous tissue or adipose tissue instead of heart muscle tissue, in the right ventricle. Thus, the right ventricle loses its function of contraction and relaxation. The fibrous or adipose tissue that replaces the myocardium will also have consequences on the heart's electricity, often appearing. Arrhythmogenic right ventricular dysplasia is also called right ventricular cardiomyopathy. Article content\n \n \n .
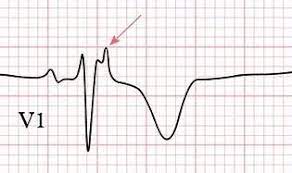
ro or from the SfatulMedicului mobile application (iOS, Android)\n . These are:\r\n\r\n. Conservative stage. You have no symptoms, but you may experience arrhythmias during physical exertion. The test results are normal and there is still no evidence of a right ventricular pathology.
2. The electric stadium. It increases the risk of having malignant ventricular arrhythmias and therefore the risk of cardiac arrest and death. Abnormal heart rhythms can be highlighted by performing an electrocardiogram. 3.
The structural stage. The structure of the myocardium begins to be visibly altered, and the risk of ventricular arrhythmias increases considerably. Imaging tests such as these will highlight structural changes in the right ventricle. Doctors encounter this pathology especially among teenagers and young adults. Arrhythmogenic right ventricular dysplasia is a frequent reason why young athletes go into cardiac arrest.
Studies say that it is more common among men. Worldwide, arrhythmogenic dysplasia affects 1 in 1000 to 5000 people. It can occur in completely healthy patients, with no personal or family history of heart disease. Although the symptoms given by the condition may be absent at the beginning, the risk of arrhythmias is present from the first modification of the myocardium. During the evolution of the disease, symptoms such as:\r\n\r\n.
Being the severe consequence of the pathology, arrhythmias are often the first sign of it. Irregular heart rhythm originates in the right ventricle and is malignant, which means it carries an increased risk of death. is the most common such arrhythmia, affecting up to 77% of individuals with arrhythmogenic right ventricular dysplasia. • Supraventricular arrhythmias. These originate in the atria and are less dangerous, rarely fatal.
• , that feeling of fast and irregular heartbeats, given by arrhythmias\r\n. The average age of diagnosis is usually before 40 years. Approximately 60% of patients diagnosed with this disease have a genetic mutation. Researchers have identified at least 13 genes that can have mutations causing arrhythmogenic dysplasia. These abnormal genes will alter the proteins involved in the formation of heart muscle tissue.
Thus, the muscle fibers will lose their connection and separate, being replaced by another tissue. Although it is not a direct causative factor, family history is present in 30% to 50% of cases of arrhythmogenic dysplasia. For this reason, the 1st and 2nd degree relatives of the diagnosed patients must be checked in time, through cardiological screening tests, even in the absence of symptoms. Two models of inheritance of this pathology have been discovered:\r\n\r\n. One of the parents has the genetic mutation.
Studies say that in these families, all members will have a 50% chance of acquiring the condition. The parent with the mutated gene is not necessarily symptomatic, but only a carrier of the gene, which he passes on. • Autosomal recessive. For a child to develop the disease, both parents must have the mutated gene, without being symptomatic or diagnosed in turn. This form is less common.
Arrhythmogenic right ventricular dysplasia can also have other causes such as:\r\n\r\n. The diagnosis of arrhythmogenic dysplasia will be established if you meet a combination of certain criteria, such as:\r\n\r\n. In some cases, genetic tests can also be recommended. Tests that will help confirm the diagnosis include:\r\n\r\n. Thus, treatment options for these patients include:\r\n\r\n.
• Antihypertensive drugs such as diuretics or beta-blockers, which ease cardiac effort. • Anticoagulant drugs, to prevent thrombosis\r\n. The interventional cardiologist will minimally invasively penetrate into the right ventricle, in order to remove the focus of the arrhythmia. • Implantation of a defibrillator, for patients at risk of cardiac arrest. • Heart transplant.
In the absence of the effectiveness of other treatments, patients become candidates for heart transplantation. Only between 2% and 4% of these patients will reach this option. Treatments can be combined to form the best option. During the evolution of the disease, the doctor can modify the treatment scheme multiple times. Patients below will have to have regular blood tests, in order not to exceed the dose.
Based on the analyses, the doctor will adjust the dose so that the risk of bleeding does not occur. Radiofrequency catheter ablation is an effective procedure for most patients. However, in 60% of cases, the arrhythmias will reappear due to the formation of another arrhythmic focus. The procedure can be repeated, but it becomes complicated when many such ablations are needed. Arrhythmogenic right ventricular dysplasia is a not very common pathology, encountered and diagnosed especially in young people.
Although it is a structural defect, cardiac function is often preserved at first, but there is a risk of malignant ventricular arrhythmias. If you have relatives with this diagnosis or if you experience palpitations and other signs of arrhythmias, do not hesitate to go to the doctor, to avoid severe consequences. Bibliography\r\n\r\n\n\n \n \n\n \n \n \n\n \n \n . ILIESCU (in the FUNDENI Hospital)\n \n \n . ILIESCU (in the FUNDENI Hospital)\n \n \n .
university. .
Source : sfatulmedicului.ro
Views : 1129
Popular Article
- (photo) Nude becomes art.
Posted: 2018-03-17, 9809 views.
- The harmful effects of air conditioning on the skin
Posted: 2017-06-08, 8518 views.
- 3 causes of dyed hair discoloration
Posted: 2017-06-15, 8402 views.
- Why early puberty occurs in girls: symptoms, favors, diagnosis and treatment
Posted: 2017-10-24, 8242 views.
- Good or bad skin treatments in the hot season
Posted: 2017-06-07, 7975 views.
Recommendations
- (photo) Nude becomes art.
Posted: 2018-03-17, 9809 views.
- The harmful effects of air conditioning on the skin
Posted: 2017-06-08, 8518 views.
- 3 causes of dyed hair discoloration
Posted: 2017-06-15, 8402 views.
- Good or bad skin treatments in the hot season
Posted: 2017-06-07, 7975 views.
- Risks of practicing sports on hot days
Posted: 2017-06-12, 7547 views.
 4 effective ingredients in the fight against acne.
4 effective ingredients in the fight against acne. How to get rid of hiccups fast
How to get rid of hiccups fast The wheat bran diet: the secret of lost pounds as if by magic
The wheat bran diet: the secret of lost pounds as if by magic The recipe that will sweeten your soul this weekend!
The recipe that will sweeten your soul this weekend!  Is it dangerous or not to refreeze meat after thawing it?
Is it dangerous or not to refreeze meat after thawing it?  The unusual sign of diabetes indicated by saliva.
The unusual sign of diabetes indicated by saliva. What to drink to boost your immune system.
What to drink to boost your immune system. 10 foods that help you never age.
10 foods that help you never age. What actually happens in your body if you drink a cup of coffee for breakfast
What actually happens in your body if you drink a cup of coffee for breakfast 5 surprising benefits of chia seeds
5 surprising benefits of chia seeds